Thanks to advances in medical technology, breast cancer and other breast issues can now be detected at an early stage, which is key for successful treatment and recovery. Before you can decide which would be the best diagnostic test for you, it is essential that you understand the differences between the options. This article will provide a comprehensive overview of the different tests available for diagnosing potential issues with the breasts: ultrasound, mammogram, and MRI scans.
It is important to note that a breast ultrasound, mammogram or MRI scan cannot diagnose all breast problems or cancer. Your doctor may recommend additional practices as part of your screening process such as physical examination and blood work. In some cases further investigation may be needed in order to determine if further treatment is needed. Finally, each of these techniques provides individual benefits and drawbacks so it is important to discuss any concerns with your doctor before deciding on a specific examination method.
Breast Ultrasound
When it comes to breast imaging, understanding the differences between the imaging methods can be key in detecting and diagnosing any abnormalities. In this guide, we'll look at what a breast ultrasound is, how it is used and how it differs from mammogram and MRI.
This guide will provide an understanding of how a breast ultrasound works and how it can be used by medical professionals.
What is a Breast Ultrasound?
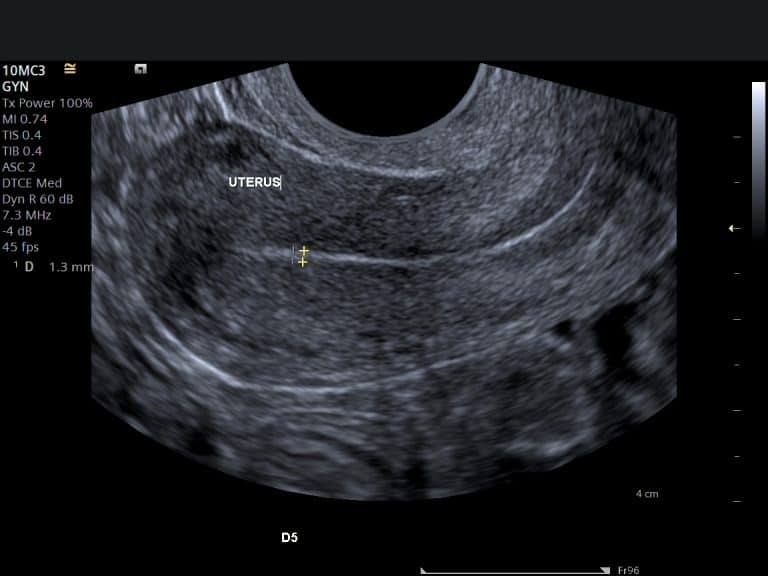
A breast ultrasound, also referred to as a sonogram or ultrasonography, is an imaging procedure used to examine the anatomy and physiology of the breast. It uses high-frequency sound waves sent through a special device (called a transducer) that generates images. It is most commonly used to detect any abnormalities in the structure of the breasts such as cysts, masses and lumps.
During a breast ultrasound, the transducer sent through the patient’s skin emits sound waves and senses them as they bounce off structures inside the body creating visual images on computer monitor. These images are assessed by specially trained radiologists who can then determine if any abnormalities exist which may require further investigation using other imaging techniques such as mammograms or MRIs.
Aside from assisting in detection of possible breast cancer pathology, breast ultrasounds can also be used to:
- Assess changes in existing lesions
- Monitor for changes following treatment for cancer
- Track implanted seeds during brachytherapy
- Assess potential complications from implants
- Evaluate ultrasound-detected lesions that cannot be seen on mammograms
Ultrasound waves are safe, painless and non-ionizing – meaning they do not carry radiation (such as x-rays) which has associated risks including an increased cancer risk over time. Thus, ultrasound offers an important tool in medical diagnosis.
What are the Benefits of a Breast Ultrasound?
A breast ultrasound is a safe and painless imaging test that uses sound waves to create pictures of the inside of the breast. It can help diagnose lumps, suspicious masses, and cysts in the breast tissue, as well as other conditions such as abscesses and tumors. Breast ultrasound is sometimes used along with mammography and MRI to provide additional information about any suspected abnormality in the breasts.
Benefits of breast ultrasound include:
- It can spot abnormalities too small for a mammogram to detect, such as early cancers or benign cysts. It is also useful for evaluating dense tissue that is difficult on a mammogram (e.g., in younger women).
- Ultrasound doesn’t use radiation like a mammogram or an MRI.
- It can detect small changes over time more easily than other imaging techniques.
- It can more easily evaluate cysts—which are fluid-filled sacs—in comparison to a mammogram in which they may look like solid masses.
- Ultrasound exams are quick and noninvasive, taking only about 15 minutes from start to finish.
- Ultrasound tests do not require contrast dye, which some people have difficulty tolerating or are allergic to it but might be necessary for an MRI exam.
How is a Breast Ultrasound Performed?
Breast ultrasound is the use of high-frequency sound waves to create a detailed image of the breast tissue. The breast is scanned in real time, allowing the doctor, radiologist or technician to observe the area’s movement and structure as they look for abnormalities.
The ultrasound technician will first apply a clear gel to the surface of your breast. This helps create an effective contact between your skin and the transducer probe that produces sound waves. An ultrasound transducer passes through a wand-like device over your breast, sending sound wave signals that reveal a three-dimensional picture of inside your body. You may be asked to hold your breath while images are taken during certain moments.
The entire procedure is painless and noninvasive, taking anywhere from 15 minutes up to an hour depending on the size of each individual’s breasts and any additional pictures requested by the doctor or specialist. Patients typically experience no discomfort during this procedure as it does not involve radiation nor does it cause any harm or damage to cells in its process of imaging.
Who Should Have a Breast Ultrasound?
Breast ultrasounds are used by doctors to help determine if any suspicious areas detected on mammograms require a biopsy. This test, considered safe and noninvasive, is often recommended for women with dense breasts because mammograms may be less reliable in detecting abnormalities in dense tissues. In addition, breast ultrasound is often recommended for women who experience breast pain or tenderness that don’t have a readily identifiable cause, as well as those who have unusual lumps or cysts such as fibroadenomas.
It’s important to note that breast ultrasound cannot detect certain types of cancer and can produce false positive results. Since the test doesn’t view the tissue from different angles like a mammogram does, some smaller cancers may not show up on an ultrasound. Those with an increased risk of breast cancer (a family history or personal history of precancerous conditions) should talk to their doctor about having regular mammograms rather than relying solely on ultrasounds for monitoring purposes.
Mammogram
A mammogram is used to detect breast cancers and other abnormalities in the breast tissue. It is used as the primary screening tool for breast cancer and is recommended for women over the age of 40. Mammograms use X-rays to create an image of the breast tissue which can then be used to detect any abnormalities.
This article will provide a comprehensive guide to understanding the differences between a mammogram, ultrasound and MRI.
What is a Mammogram?
A mammogram is a type of X-ray of the breasts that can detect breast cancer and other types of abnormalities. Mammograms are the most common screening for breast cancer in women over the age of 40, but they may also be recommended for certain younger women who have an increased risk of developing breast cancer.
Mammograms work by sending low-dose radiation through the breast tissue to create images that doctors can use to look for any signs of disease. While mammograms can detect smaller lumps or tumors than might be detectable during a physical exam, they are also more sensitive so false positives (abnormalities that turn out not to be cancer) occur more often.
During a mammogram, you’ll typically be positioned between two plates which will flatten your breasts before an X-ray machine takes images from two angles. Mammograms are generally not painful, but some women may find it uncomfortable when the technician flattens their breasts for imaging. Afterward, all images will be reviewed by a radiologist who will compare any suspicious areas with your past mammograms in order to determine if any follow up is needed.
What are the Benefits of a Mammogram?
Mammograms are a form of imaging that uses low dose x-ray beams to detect changes in the breast tissue. They are an important screening tool for women to help identify any potential health risks in the early stages, when treatment is more successful. The goal of a mammogram is to detect breast cancer before it is palpable or visible on an image, which increases your chances of early diagnosis and timely treatment.
Some of the primary benefits of having a mammogram include:
- Increased chances of detecting breast cancer earlier when it may be treatable. Early detection would reduce the risk of advanced stages and more aggressive treatments.
- Enhanced accuracy in evaluating irregular densities or masses that cannot be detected by physical examination alone.
- Better examination and classification screening procedures due to the high resolution images created from a mammogram.
- Reduced, but not eliminated, the need for additional diagnostic imaging tests such as ultrasounds or biopsies if results show no abnormalities on a mammogram.
- Opportunity for your doctor to track changes in your breasts over time through follow up visits and subsequent screenings every 1 – 2 years (depending on your current age and personal health history). Periodic evaluations can also allow for earlier detection if any health changes occur between screenings.
How is a Mammogram Performed?
A mammogram is a type of imaging used to screen for and diagnose breast cancer. It uses low-dose x-rays to create a three-dimensional image of the breast that is analyzed for any signs of abnormal changes. Regular screening mammograms can help decrease mortality from certain types of cancers by detecting them at an earlier stage when treatment is more successful.
To perform a mammogram, a technologist will position the patient's breast between two plates that are connected to an x-ray machine. Pressure may be applied to reduce the amount of radiation exposure and flatten the breast’s tissue for examination. Typically, two images are taken from opposite sides in order to have different angles from which any abnormalities can be evaluated. The traditional mammogram process can take 15–20 minutes and may cause slight discomfort due to being pressed between the plates during the procedure.
However, newer techniques such as 3D Tomosynthesis (also called Digital Breast Tomosynthesis or DBT) provide improved visualization that allows doctors to better assess suspicious areas compared with traditional 2D imaging. DBT makes it possible to pinpoint abnormalities with more accuracy because it takes multiple images in thin slices, providing more detailed insight into your results than traditional mammography alone was able to provide before its development in 2011. This form of imaging takes up to 20 seconds longer than a regular mammogram but reduces false positive results and improves diagnostic accuracy overall.
Who Should Have a Mammogram?
Mammograms are an important part of breast cancer screening and detection. Mammograms are recommended for women age 40 and over on an annual basis, or more often if there is a family history of breast cancer or other factors that put them at increased risk for the disease. This recommendation is based on numerous studies showing the clear benefits of mammography in reducing death from early-stage breast cancer in women.
The American College of Radiology (ACR) also recommends that women who have had borderline mammogram results discuss further testing options with their healthcare provider. This includes, but is not limited to, follow up mammograms or additional tests such as ultrasound and MRI, which may be recommended depending on a patient’s age, symptoms, family history and other risk factors. These additional tests can provide a clearer picture when studying a suspicious area or diagnosing a lesion that can’t be seen by routine digital mammography.
For younger women experiencing symptoms or those at higher risk due to prior treatment like radiation therapy or hereditary BRCA1/2 gene mutations who wish to receive yearly breast imaging as precautionary screening by medical practitioners, an MRI may be considered instead of regular mammograms at their own discretion.
MRI
Magnetic Resonance Imaging (MRI) is a noninvasive imaging technique used to take pictures of the inside of the body. It is often used for diagnosis of breast cancer and other breast abnormalities. MRI is often used in combination with mammography and ultrasound to get a more complete picture of the breast.
Let's explore the advantages and disadvantages of MRI.
What is an MRI?
Magnetic resonance imaging (MRI) is a widely used diagnostic imaging procedure that is utilized to view images of the internal structure of the body. MRI scans can be used to diagnose disorders and injuries, particularly musculoskeletal disorders and injuries, by providing detailed pictures of soft tissues, muscles, cartilage and organs within the body.
During an MRI, radio waves are induced into the body by a powerful magnetic field which then produces signals that a computer interprets as cross-sectional images.
MRI scans safely produce highly detailed cross-sectional images of various areas within the body with no use of radiation. These scans allow doctors to accurately assess health conditions from multiple angles instead of relying on static 2D X-ray images which can decrease the accuracy in diagnoses.
MRI is typically used for diagnosing diseases and trauma injuries in brain and spinal cord along with breast cancer screening and evaluation for vascular diseases. Because MRI does not involve any radiation exposure it can be safely repeated if necessary, even multiple times in same day for long exams such as for spine or knees. The imaging aspect uses no contrast media or ionizing radiation so it’s also much less dangerous than other methods such as radiography or CT scan which involve radiation exposure.
What are the Benefits of an MRI?
Magnetic resonance imaging (MRI) of the breasts is a non-invasive procedure that uses no radiation. It is especially useful for women who cannot have a mammogram due to a surgically implanted medical device, such as a breast implant, defibrillator or drug infusion port; women who have dense breast tissue and may be at high risk for cancer; or women whose soft tissue and/or calcifications have been detected.
The benefits that MRI provides over other imaging tests include: providing detailed 3D images in addition to 2D images; being able to detect tumors in poorly lit areas where there might not be any visual evidence of cancer on an image; and identifying the exact size, shape and location of cancerous tumors. Because MRI produces highly detailed images in multiple planes, it is better at detecting small changes than mammography or ultrasound, making it particularly valuable for women with heterogeneously dense breasts.
MRIs are also helpful in determining whether a suspicious area requires further evaluation or is simply benign. An MRI scan can provide valuable information about the extent of the cancer when diagnosing invasive cancers to help decide on more effective treatment plans specifically tailored to the patient’s unique circumstance.
How is an MRI Performed?
Magnetic resonance imaging (MRI) is a medical imaging modality used to create detailed images of the body’s organs and tissues. It is a non-invasive procedure that does not expose the patient to radiation. An MRI uses powerful magnets, radio waves, and computers to produce 3D or 2D pictures of organs and body structures.
An MRI works by placing strong magnetic fields around the area that is being scanned. Then, radio frequency pulses are sent through the patient’s body, creating signals from different tissue types. The signals are then interpreted by a computer to create an image on a monitor or printed off for further diagnosis.
To aid in creating the images, contrast agents may be used to further highlight areas that require extra detail or clarity. A contrast agent is a special dye that is injected into the bloodstream prior to having an MRI. This dye helps identify areas of inflammation or injury that may be difficult to detect otherwise.
Prior to an MRI scan, you will be asked questions about your health history and any allergies you may have as well as providing your doctor with information regarding any medications you may be taking so they can adjust them based on their experience with MRI scans. Additionally, most people undergo an X-ray beforehand in order for doctors to get a baseline reading prior to starting with an MRI scan as well as estimating how much contrast agent will need to be used in order for optimal imaging results during the scan itself.
Who Should Have an MRI?
MRI is a different technology than mammograms and ultrasounds, and it can provide more detailed information about breast tissue, particularly for those with dense breasts. For instance, an MRI may be more effective in detecting cancers in younger women since their breast tissue is generally denser than that of an older woman. Additionally, unlike a mammogram or ultrasound which employs radiation to view the breast, MRI technology uses powerful magnets to take pictures of the inside of your body — meaning that there are no risks from radiation exposure associated with this type of medical imaging.
For this reason, MRI is a valuable additional tool for women at higher genetic risk for developing cancer due to known mutations in BRCA1 or BRCA2. Other factors which warrant consideration for using MRI in addition to mammography or ultrasound include a strong family history of cancer, prior prediagnostic findings not seen on imaging [such as calcifications] which are suspicious for cancer and a personal history of first-degree relative diagnosed with premenopausal breast cancer.
One important distinction between diagnosis by mammogram vs MRI is that MRIs often identify benign lesions thought to be suspicious on examination (which physicians then follow up on with biopsies) while mammograms may miss other types of benign lesions due to their size or location making them difficult to detect in the standard two-dimensional view obtained by this exam. While physical examination remains an important tool in grading the risk factors associated with specific lesions on MRIs — coupled with targeted review by a physician trained in reading and interpreting these images — can help assure disease stratification allowing doctors and patients make informed decisions when understanding outcomes and corresponding treatments options.
Conclusion
Ultimately, breast ultrasounds, mammograms, and MRIs are all important tools for assessing a woman’s risk of developing breast cancer. Each of these processes offers unique advantages and drawbacks which must be taken into account when making a decision about which form of imaging to use.
Mammograms can detect suspicious lumps that may be indicative of cancers at an early stage, while ultrasounds are best used to better define the shape and extent of the abnormality. MRI can be used to assess the extent of a tumor or to determine whether the cancer has spread beyond the original location.
When combined, these three forms of imaging provide women with a powerful arsenal in their fight against breast cancer. By understanding how each type of imaging works and identifying which is best for their individual needs, women can make informed decisions about which tests they choose and ensure they receive optimal care if they suspect or are diagnosed with breast cancer.
Content Information
We review all clinical content annually to ensure accuracy. If you notice any outdated information, please contact us at info@iuslondon.co.uk.
About the Author:

Dr. Mohammad Jalaleddin (GMC number: 7729988) is an internationally-trained physician who earned his medical degree from Tishreen University in Syria in 2005. He completed his specialization in diagnostic radiology in 2009, followed by a Master's degree in 2011, which focused on the radiological alterations of bone grafts. Dr. Jalaleddin has worked as a radiologist in various hospitals and clinics, developing significant expertise in ultrasound and MRI scans. He has extensive experience in performing a wide range of ultrasound examinations, including breast, abdominal, pelvic, and vascular studies. In 2017, he moved to the UK and completed the requalification process with the General Medical Council (GMC). Since March 2021, he has been a part of the Imperial College Healthcare NHS Trust. Dr. Jalaleddin is a member of the General Medical Council (GMC) and the British Medical Ultrasound Society (BMUS).