Follicular tracking, also known as follicle monitoring, is an important part of fertility care and treatment. It involves using ultrasound imaging to track the growth and development of ovarian follicles during a menstrual cycle. The purpose of follicular tracking is to monitor follicle growth, identify the optimal timing of ovulation, and guide decisions about fertility interventions like timed intercourse, intrauterine insemination (IUI), or in vitro fertilization (IVF).
What are Ovarian Follicles?
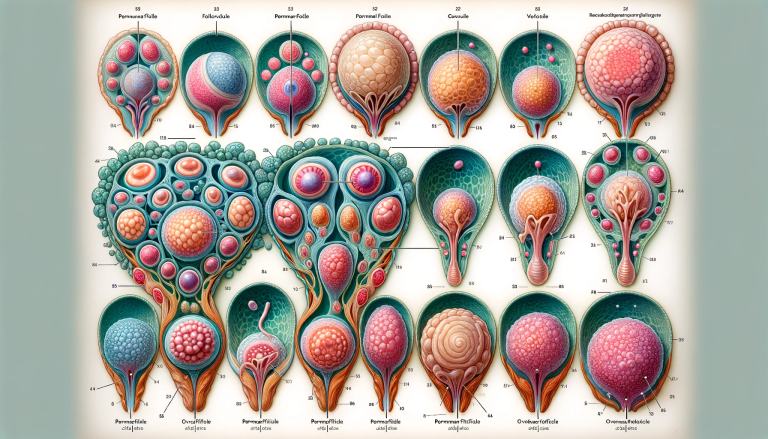
- Ovarian follicles are small sacs in the ovaries that contain immature egg cells (oocytes)
- At birth, women have a lifetime supply of several hundred thousand follicles. This number declines with age through a process called atresia.
- During each menstrual cycle, a cohort of follicles is recruited to start growing and developing. Typically only one follicle will reach full maturity and release an egg.
The Follicular Phase of the Menstrual Cycle
Follicular tracking focuses on the first half of the menstrual cycle, known as the follicular phase:
- Menstrual Phase (Days 1-5) - The menstrual period sheds the uterine lining if no pregnancy occurs in the previous cycle. Hormones FSH and LH are low.
- Follicular Phase (Days 6-14) - Under stimulation from FSH, a group of follicles start growing. Typically 1 follicle becomes dominant and continues maturing. Estrogen levels rise.
- Ovulation (Day 14) - The dominant follicle ruptures and releases its mature egg. LH and estrogen surge triggers ovulation.
During this follicular phase, regular ultrasound scans can track the growth of ovarian follicles and identify the pre-ovulatory follicle that will release an egg.
Why is Follicular Tracking Important?
Follicular tracking serves several important purposes:
- Pinpoint the timing of ovulation more precisely
- Guide fertility medication dosage and timing
- Reduce the risk of multiple pregnancies with fertility treatment
- Detect issues like low ovarian reserve or ovulation disorders
- Time intrauterine insemination or egg retrieval procedures optimally
By closely monitoring follicular development each cycle, the most fertile days can be identified more accurately. This maximizes the chances of conception through timed intercourse or infertility treatments.
How Does Follicular Tracking Work?
Follicular tracking involves using transvaginal ultrasound scans to visualize and measure ovarian follicles during development. Pelvic ultrasounds use high-frequency sound waves to create images of the reproductive organs. A probe is inserted into the vagina to get closer to the ovaries for better resolution.
At each ultrasound scan, the number, sizes, and locations of visible follicles are measured and recorded. The pattern of growth from baseline provides important information:
- Number of Follicles - Typically less than 10 follicles develop together initially. Too many follicles could indicate potential complications.
- Follicle Size - The diameter indicates maturity. Follicles grow 1-3 mm per day. Mature eggs ovulate from follicles >18-20 mm.
- Dominant Follicle - One follicle becomes dominant and continues growing while others stop maturing. This will release the egg.
- Endometrial Lining - The thickness of the uterine lining is measured to ensure adequate growth.
- Ovulation - Follicles suddenly collapse after ovulation as the egg is released. Fluid or blood is sometimes visible.
Depending on the clinical goal, follicular tracking scans are generally performed every 1-3 days until ovulation is detected. The series of ultrasound measurements allow the lead follicle and ovulation to be identified.
When is Follicular Tracking Started in a Cycle?
The start day for follicular tracking depends on whether the woman has regular cycles and whether fertility medications are used:
- Natural Cycles - Ultrasounds generally begin by cycle day 10 in ovulatory women with regular cycles. Earlier if cycles are shorter.
- Ovulation Induction - With medications like clomiphene or letrozole, ultrasounds often start on cycle day 3 to establish a baseline. Continue until ovulation.
- IVF Cycles - Tracking begins with the onset of menstrual bleeding. Frequent ultrasounds monitor follicle response to fertility drugs.
- Irregular Cycles - Unpredictable cycles may require ultrasounds from the start of menstruation to identify follicle growth whenever it occurs.
The goal is always to pinpoint the optimal ovulation day based on follicle maturity. Starting scans early enough to detect the beginning of follicle growth is important.
How Often are Follicular Tracking Scans Needed?
The frequency of follicular tracking depends on the stage of follicle development:
- Early Follicular Phase - Every 2-3 days
- Around Selection of Dominant Follicle - Every 1-2 days
- Approaching Ovulation - Daily
At critical decision points closer to ovulation, daily ultrasounds are often needed to time procedures precisely and avoid premature ovulation. The frequency balances monitoring needs with reducing visits and costs.
Some key factors that may warrant more intensive follicular tracking include:
- Use of injectable fertility medications
- History of rapid ovulation
- Irregular or unpredictable cycles
- Undergoing IUI or IVF treatment
Otherwise, every 2-3 days is typically adequate to effectively track follicle growth.
What is Monitored During Follicular Tracking Ultrasounds?
Several parameters are assessed during each follicular tracking ultrasound:
- Number of Follicles - The total number of follicles visible in each ovary.
- Size of Follicles - The diameter of each follicle is measured. Mature follicles ovulate around 18-24 mm.
- Dominant Follicle - The largest, most mature follicle that will likely ovulate.
- Endometrial Lining - The thickness of the uterine lining should reach around 8 mm for implantation.
- Ovulation - Follicles may show collapse, fluid or blood when the egg releases.
- Ovaries & Uterus - Screen for abnormalities in anatomy, fibroids, cysts etc.
Monitoring all of these parameters provides an overall picture of menstrual cycle health and how follicles are progressing each day.
Follicular Tracking Results and Interpretation
The follicular tracking results will be interpreted by a fertility specialist based on:
- Number of Follicles - Typically see less than 10 growing together initially. Too many could mean overresponse risk.
- Follicle Growth Rate - Ideal is 1-3 mm increase in size per day after reaching 10 mm. Slower growth may need medication changes.
- Dominant Follicle Size - Looking for the lead follicle to reach 18-24 mm before ovulating.
- Endometrial Lining - Should reach 8 mm thickness to be ready for implantation after ovulation.
- Ovulation Timing - Want to see ovulation around cycle day 14 if regular cycles. Later in polycystic ovary syndrome.
- Cycle Cancelation - Overresponse or underresponse to medications may result in canceling the cycle.
The follicular phase results will guide medication dose adjustments and optimal timing of procedures like IUI or egg retrieval in IVF.
Who Needs Follicular Tracking?
Follicular tracking is especially useful for patients:
- Trying to conceive and needing to time intercourse
- Using oral ovulation induction medications like clomiphene
- Undergoing intrauterine insemination (IUI) procedures
- Doing in vitro fertilization (IVF) treatments
- With irregular menstrual cycles or ovulation disorders like PCOS
- With unexplained infertility despite normal fertility testing
By precisely identifying the fertile window each cycle, follicular tracking maximizes conception chances and guides assisted reproductive procedures. It provides insight for diagnosis and treatment.
What is Antral Follicle Count Testing?
In addition to cycle monitoring, follicular tracking can also assess ovarian reserve using antral follicle counts:
- Performed at the beginning of the menstrual cycle before follicle growth begins
- Measures the number of small antral follicles visible in the ovaries
- Reflects the number and quality of remaining eggs
- Low counts may indicate diminished ovarian reserve
- Counts decline naturally with age as fertility decreases
This baseline measurement indicates fertility potential independent of the current cycle. It helps identify women who may need more tailored treatment or egg freezing at a younger age due to low counts.
Potential Drawbacks of Follicular Tracking
While follicular tracking is an invaluable fertility tool, there are some potential limitations to consider:
- Requires frequent ultrasound appointments that can be inconvenient
- Not all follicles are visible on ultrasound so results may not show complete picture
- User-dependent - operator experience impacts consistency and accuracy
- Adds significant costs if not covered by insurance
- Can be uncomfortable physically and emotionally if poor response
However, most patients feel the benefits of maximizing conceive chances outweigh any inconveniences. Understanding what to expect can help manage expectations.
What to Expect During Follicular Tracking
Here's an overview of what to expect with follicular tracking:
- Transvaginal Ultrasound - Probe is inserted into the vagina to visualize ovaries and uterus.
- Full Bladder Not Needed - Empty bladder provides clearer imaging so don't drink water before appointments.
- Pelvic Exam - The doctor may perform a brief manual pelvic exam before the ultrasound.
- Discomfort - Some women experience mild discomfort or pressure during the procedure. Speak up about any pain.
- Condom Use - Sterile coverings over the probe are standard. Do not rely on them for contraception.
- Measurements - The doctor will measure follicle sizes verbally and record measurements.
- Photos - Images are stored but typically not provided unless requested.
- Review Results - The doctor will explain follicle growth and next steps after each scan.
- Timing of Ovulation - You'll be advised on optimal timing of intercourse, IUI or egg retrieval.
Communicate any questions or concerns you have before, during or after appointments. Stay in contact between scans for any updates.
Questions to Ask About Follicular Tracking
When meeting with your doctor about follicular tracking, consider asking:
- How many follicles are developing? What sizes are they?
- Do you see a dominant follicle emerging? How big is it?
- How fast are my follicles growing each day? Is the growth pace normal?
- How thick is my endometrial lining? Is it thick enough to support pregnancy?
- When do you expect I will ovulate based on the follicle growth?
- Should I make any medication dosage changes based on the results?
- Do I need to come in for daily scans as I get closer to ovulation?
- Are my antral follicle counts in normal range for my age? Do they indicate low reserve?
- What are the next steps you recommend based on my follicle development?
Tips for Follicular Tracking Patients
Here are some tips to help get the most out of your follicular tracking:
- Track your appointments and record measurements each visit. Apps or calendars help stay organized.
- Time appointments early if possible to avoid work disruption. Weekday early mornings often work best.
- Confirm insurance coverage for follicular tracking and potential out-of-pocket costs.
- Come with a full bladder for the first scan to visualize anatomy, empty after that.
- Take ibuprofen or pain reliever before scans if you experience discomfort.
- Abstain from intercourse after instructed to avoid premature ovulation.
- Communicate any concerning symptoms like pain, bleeding or discharge promptly.
- Follow medication instructions closely and give yourself injections carefully.
- Reach out between scans with any questions or concerns about your follicular phase.
Staying on top of your cycle with follicular tracking helps set yourself up for success!
Follicular Tracking and Fertility Treatment
Follicular tracking is especially critical for guiding fertility treatments like:
Ovulation Induction Medications
- Oral medications like clomiphene citrate or letrozole stimulate follicle growth and ovulation.
- Follicular ultrasounds allow doctors to monitor response, adjust dosing, and time intercourse or IUI.
- Helps achieve ovulation in anovulatory disorders like PCOS. Also useful for unexplained infertility.
Intrauterine Insemination (IUI)
- IUI coordinates insemination right around the time of ovulation for optimal chances.
- Daily tracking determines the ideal day for the procedure based on follicular maturity.
- Ensures the semen sample is inserted when the egg is ready.
In Vitro Fertilization (IVF)
- Allows close monitoring of follicle development during injectable ovary stimulation.
- Guides dosage adjustments of gonadotropin medications to avoid under or over response.
- Timing of egg retrieval procedure is based on reaching appropriate follicle sizes.
- May cancel and freeze cycle if too few or too many follicles develop.
Follicular tracking is critical for maximizing success rates with these fertility treatments.
What Next After Follicular Tracking?
Once ovulation is detected on ultrasound, next steps depend on your fertility goals:
- Timed Intercourse - Abstain until instructed to try conceiving in the fertile window.
- Intrauterine Insemination - Return on the designated day(s) to have semen sample inserted into uterus.
- Egg Retrieval - Procedure will be scheduled for egg aspiration when follicles are mature.
- HCG Trigger Shot - An injection may be given to induce ovulation once lead follicle reaches size.
- Progesterone Testing - May monitor progesterone rise to confirm ovulation occurred.
- Pregnancy Test - Take a pregnancy test if period is late. Inform clinic of results.
Stay in close contact with your doctor's office around the time of expected ovulation and the days after. Follow all instructions for optimal chances of pregnancy.
Follicular Tracking Results and Fertility Outcomes
The response seen during follicular tracking offers clues about fertility potential:
- Normal Response - Ideal follicle growth and ovulation. Offers best prognosis.
- Low Response - Fewer follicles than expected may indicate low ovarian reserve or need medication change. Harder to achieve pregnancy.
- High Response - Excess follicles increase risk of multiples and ovarian hyperstimulation syndrome. May require canceling cycle.
- No Follicle Growth - Could mean primary ovarian insufficiency with extremely low reserve. Requires egg donor to carry pregnancy.
- No Dominant Follicle - Failure of one follicle to mature may signal ovulation disorder. Medication like clomiphene may help.
- Thin Lining - Difficulty growing adequate endometrial lining can also reduce chances of implantation and pregnancy.
The response often provides valuable insight for fertility doctors to optimize treatment moving forward. Patience and persistence is key.
Wrap Up
- Follicular tracking uses ultrasound to monitor the development of ovarian follicles during the first half of the menstrual cycle.
- It identifies the dominant follicle that will ovulate and pinpoints the optimal fertility window.
- This allows accurate timing of intercourse, insemination, or egg retrieval procedures.
- Frequency of ultrasounds ranges from every 2-3 days up to daily tracking as ovulation approaches.
- Follicular results guide fertility medication dosage changes and treatment procedures.
- Understanding what to expect during scans and asking the right questions helps maximize your chances of conception.
Follicular tracking provides invaluable insight into ovulation timing and fertility potential. Discuss implementing this important tool with your doctor to take control of your chances of getting pregnant.