Pregnancy is almost synonymous with morning sickness. It is the most common disorder of early pregnancy, affecting up to 85% in some studies. Although it is commonly used, the term “morning sickness” is incorrect for several reasons. Firstly, sickness during pregnancy can occur any time of the day and secondly, although the term refers to sickness, most pregnant women experience more nausea than sickness.
Morning Sickness – Pregnancy nausea and vomiting
The correct term for this set of symptoms is Nausea and Vomiting of Pregnancy (NVP) to differentiate the symptoms that accompany other disease states, including radiotherapy and chemotherapy. Nausea and Vomiting of Pregnancy is a mouthful and will use NVP more frequently.
Morning Sickness of pregnancy may start as early as five weeks but is well established by nine weeks. Although NVP tends to settle by week 16 of pregnancy, about 20% of women may still have these symptoms to some degree throughout pregnancy. It must be uncommon for a pregnant woman to go through pregnancy without any of these, sometimes debilitating symptoms.
Morning Sickness – Can Be a Recurring Problem!
The chance of morning sickness pregnancy recurring in the subsequent pregnancy is about 15%, and a change of partner reduces the risk of recurrence to about 10%.
Nausea and Vomiting of Pregnancy – Cause Unknown!
In spite of the condition being very common, affecting hundreds of thousands in the UK and millions across the world, the underlying causes remain a mystery. Some hypotheses are gaining ground.
- Morning Sickness is related to pregnancy Hormones. This theory is supported by the fact that nausea and vomiting is associated with pregnancy, symptoms subside with miscarriage (even following unrecognised miscarriage when no other symptoms have presented), twins cause more pronounced sickness and vomiting, and some pregnancy states with large placentas are also associated with increased NVP.
- Morning Sickness during pregnancy could be a good sign. Proponents of this theory suggest that by being sick, the pregnant woman is removing toxic substances contained in some foodstuff that could be harmful to the very early fetus, still in the early stages of organ formation. Studies across societies show that the association between diet and morning sickness support the idea that sickness serves a protective function against potentially harmful substances at such a vulnerable stage of development. Animal products-based foods are more likely to be associated with morning sickness than plant-based foods.
- Thyroid function and disturbance in pregnancy. It is established that the Thyroid gland is affected in some way by pregnancy hormones because they share some molecular structures and mechanisms of action (receptors). There is no clear evidence of the thyroid gland inducing morning sickness, although morning sickness can worsen the effects of thyroid function changes in early pregnancy.
- An adaptation process. It is well documented that women who experience less of NVP are at higher risk of miscarriage. So NVP may be an adaptation mechanism that protects the baby in some way.
- It is unclear why the female fetal sex is associated with a severe form of NVP – “hyperemesis gravidarum”.
- Other theories abound
Mother & Baby Consequences of NVP
For most pregnant women, NVP settles between weeks 12 and 16 without real hardship for the woman. For about 1 – 2% of women, the sickness is bad enough to warrant hospitalisation and treatment with intravenous fluids and antiemetic injections.
The effects of severe sickness, more than five times a day, associated with failure to drink or eat adequately can have severe consequences for the mother’s well-being. Extreme weakness, dehydration, and weight loss follow. The clinical term “hyperemesis gravidarum” refers to this group of women who need hospital treatment and support.
Ketones, a by-product of fat metabolism passed in the urine, are a sign that the woman is metabolising fat instead of carbohydrate as her source of energy. This heralds a degree of fluid and nutritional imbalance as a result of a sickness that if untreated, can be serious to the woman. The more ketones detected in the urine, the more serious the condition. Usually, the baby is unaffected except in extreme of cases.
Urea, an essential marker of kidney function, may be altered, indicating poor clearance of waste products from the pregnant woman due to dehydration. This is why fluid intake and replacement are so important.
In rare circumstances, especially when sickness has lasted more than three weeks, neurological complications can arise due to poor nutrition and low vitamin B series.
Not only are their physical effects, but also psychological impacts can be severe. A few women may be forced to consider terminating a pregnancy after all else fails. It is thought women with severe vomiting in pregnancy are more prone to depression.
How to Avoid Worsening Nausea and Sickness
There are a number of steps a woman can take to prevent the situation from worsening. First is to know that in all probability, this is a transient situation. That sickness does not reflect on the status of the baby.
Some of the following actions have been shown to be helpful and should be tried before medication with the view of averting the necessity of hospital admission.
The majority of women do not need any form of medication. Our advice is to drink small amounts of fluids more frequently so that the stomach is not distended, but the total fluid and nutrient intake is adequate. Spicy foods and coffees may further irritate the stomach to precipitate sickness. It is important to realise that the stomach of pregnant women does not empty as quickly as in the non-pregnant state – which may contribute to the problem.
The affected woman will be advised to rest as much as possible and avoid trigger events such smells that are likely to set off nausea or vomiting.
Diagnosis & treatments
Diagnosis is relatively easy and straightforward, based on a history of nausea and vomiting in a pregnant woman. However, not all nausea or vomiting in pregnancy is due to pregnancy. It is important, therefore, that women report worsening, persistent vomiting, especially when associated with headaches, extreme weakness, diarrhoea, and fevers.
All women with nausea and vomiting need support and understanding because of the disruption the condition is bound to have on their social, economic and psychological states. Reassurance and words of comfort may be all that is necessary because of the transient nature of NVP.
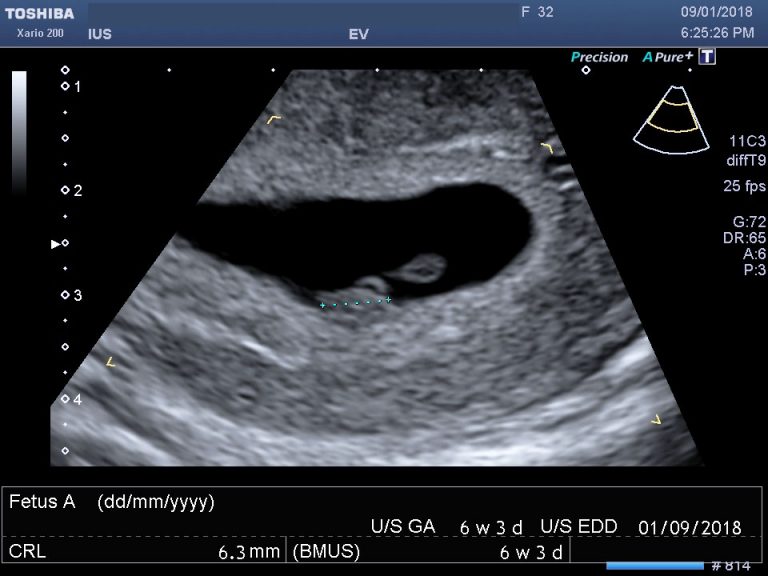
Ultrasound scans and blood tests
Investigations will include urine and blood tests to assess the degree of biochemical and nutritional disturbances. The results will inform the strategies to be adopted in caring for sick woman. The same tests are used to assess the success of treatment and recovery.
Pelvic ultrasound is useful in confirming the gestation, number of babies and other potential pathologies. A molar pregnancy has specific and characteristic ultrasound features which easily identify the existence of the condition. An early scan will identify a twin pregnancy; multiple pregnancies are associated with the more serious type of NVP. Although women often seek baby scans for reassurance of their babies’ well-being, there is really no value of repeated scans at this early stage.
Alternative Therapies
There is considerable evidence that Ginger extract is effective in managing NVP but may be insufficient for the more serious hyperemesis.
P6 acupressure point stimulation or pressure on the wrist is efficacious in managing NVP. The same technique has also recently been shown in controlled studies to be effective in other forms of nausea and vomiting following major surgery. A quick search on the internet will show a wide range of P6 acupressure antiemetic wrist devices with a wide price range – similar sorts of items used for motion or sea sickness.
Supplements, including folic acid and Vitamin B6, are part of general advice and are part of many protocols following evidence showing reduced severity of NVP among users.
Medication
Because of the Thalidomide tragedy, families, and doctors are extremely cautious about medicines in pregnancy, especially in the first trimester.
When simple measures are not enough, antihistamines such as promethazine (phenergan), procloperazine (stemetil) and metoclopramide may be prescribed. If symptoms do not improve, doctors will decide on the next measures, including additional medication and route of administration, for example, by injection. Rectal administration of anti-emetics avoid is convenient because treatment is self-administered, avoids the injections and does not precipitate sickness.
When Vomiting becomes Serious
Admission into the hospital will depend on several factors, especially if the vomiting is intractable and a woman shows signs of dehydration. The usual assessment methods include taking a history of the number of times a woman has been sick, whether she can eat or drink and how medication has been tried previously. Any of the following symptoms warrant immediate medical assessment – vomiting blood, fainting or loss of consciousness, yellowing of eyes, disorientation, palpitations and shortness of breath, painful micturition or scanty dark urine, and fever.
If the examination and testing confirm dehydration and ketones in the urine, the treatment plan may include antihistamine or other types of injections to stop the vomiting whilst the restoration fluids are intravenous. In most cases, the vomiting subsides within 24 to 48 hours. Once the woman can drink and eat and can tolerate oral medication, she may be discharged. It is essential to avoid relapse and complications. Nutritional advice and vitamin B supplements may be required.