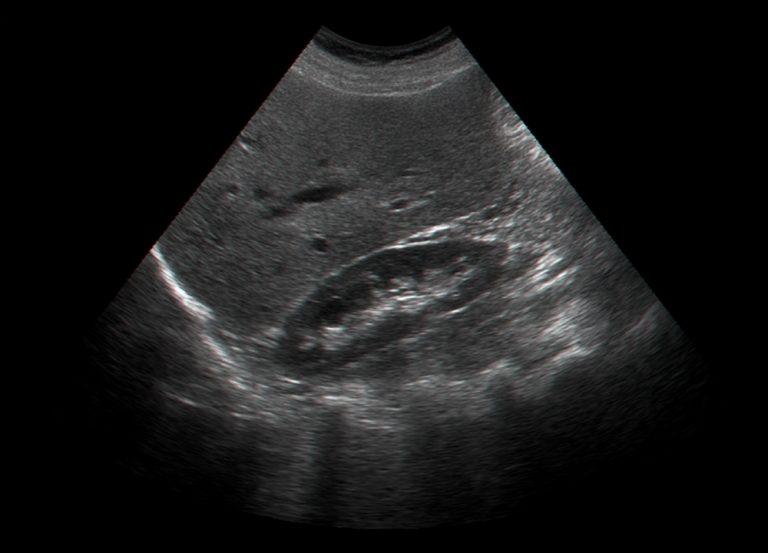
Testicular ultrasound, also known as scrotal ultrasound, is an important imaging modality used to evaluate the testicles and scrotum. It utilizes high frequency sound waves to produce images of the testicles, epididymis, and scrotal contents. Testicular ultrasound is a quick, non-invasive, and inexpensive way to help diagnose diseases and conditions of the scrotum. It is often the first imaging test ordered when a scrotal abnormality is suspected.
Testicular ultrasound is indicated for a variety of reasons including scrotal pain, swelling or masses, trauma, male infertility, cryptorchidism, and screening high risk patients. It can help differentiate between intratesticular and extratesticular processes and characterize masses as solid or cystic. The high resolution images allow detailed evaluation of the testicular parenchyma and paratesticular structures. Ultrasound is excellent at detecting testicular cancer at an early stage as well as evaluating spermatoceles, varicoceles, epididymitis, orchitis, and torsion.
Anatomy and Physiology
Anatomy
The scrotum is a sac of skin and fascia located behind the penis that contains the testicles, epididymis, and lower portions of the spermatic cord. It helps regulate the temperature of the testicles.
The testicles are a pair of oval organs contained within the scrotal sac that produce sperm and hormones. They are surrounded by a tough fibrous capsule called the tunica albuginea. Internally, the testicles contain seminiferous tubules where sperm develop.
The epididymis is a comma-shaped structure located along the posterior surface of each testicle. It is the site where sperm mature and are stored. The head, body and tail of the epididymis can be identified on ultrasound.
The spermatic cord contains nerves, blood vessels, lymphatics, and the vas deferens. It ascends through the inguinal canal to attach the testicle to the abdomen.
Blood Supply and Innervation
The testicular arteries arise from the abdominal aorta and supply blood to the testicles. The pampiniform plexus is a network of veins that help regulate testicular temperature. The testicular veins ultimately drain into the inferior vena cava.
The testicles are innervated by both sympathetic and parasympathetic fibers of the autonomic nervous system. The genitofemoral nerve supplies sensation to the scrotal contents.
Hormonal Function
The testicles are responsible for the production of the male hormones testosterone and androsterone. Testosterone stimulates the development of male secondary sex characteristics and reproductive tissues. The levels are controlled through the hypothalamic-pituitary-gonadal axis.
Indications
There are many reasons why a testicular ultrasound may be ordered by a physician:
- Palpable mass, pain or swelling: To evaluate any palpable abnormalities of the scrotum and determine if they are inside or outside the testicle. While most scrotal masses are benign, any mass has malignancy potential until proven otherwise.
- Follow up of known mass or lesion: To monitor a known lesion for changes in size or appearance. Serial ultrasounds are often used for testicular tumor surveillance.
- Trauma: Assessment for rupture or hematoma after scrotal trauma. Ultrasound is more sensitive than physical exam for detecting testicular rupture.
- Infertility evaluation: To check for abnormalities like varicoceles that may be contributing to male factor infertility. Scrotal ultrasound is part of a standard infertility workup.
- Cryptorchidism: Evaluation of suspected undescended testis which are at higher risk for developing malignancies.
- Screening in high risk patients: Ultrasound screening may be done in patients at high risk for testicular cancer, such as those with a history of undescended testes, prior germ cell tumor, or genetic conditions like Klinefelter's syndrome.
Preparation
No special preparation is required for a testicular ultrasound. The scrotum should be shaved if necessary to allow close contact between the transducer and skin surface. Shaving should be done shortly before the exam to prevent stubble that could interfere with imaging.
A generous amount of warm ultrasound gel is used to fill the space between the transducer and scrotum. This allows for clear visualization without compression of the delicate structures. Some gentle compression may be applied to evaluate intratesticular blood flow.
Procedure
Patient Positioning
The patient is placed in a supine position with the penis draped upward toward the abdomen. A towel is sometimes placed between the legs for privacy and warmth. The scrotum is supported by a towel or cloth placed beneath it. Having the patient bend his knees and rotate hips outward allows the scrotum to lay flat for optimal imaging access.
Transducer Selection
A high frequency linear transducer, typically between 7-12 MHz, is used for testicular ultrasound. The high frequency provides excellent resolution of the superficial testicular anatomy. Lower frequencies may be utilized for deeper evaluation of the spermatic cord.
Scanning Approach
A systematic scanning approach is important to fully evaluate both testicles and adjacent structures. Each testicle is imaged in both transverse (short axis) and longitudinal (long axis) planes from superior to inferior poles.
The exam begins with transverse images to get an overview of the testicular size, shape and echogenicity. The epididymis is visible along the posterior surface of the testicle. Next, longitudinal images in orthogonal planes are obtained to follow the long axis of the testicle and document the full extent of any lesions.
Doppler ultrasound can be used to assess blood flow within the testicles. Power Doppler helps identify testicular perfusion, while spectral Doppler quantifies flow velocities. Loss of vascular flow is an important indicator of testicular torsion.
Both testicles are scanned in multiplanar views to allow side-by-side comparisons. Clinical correlation to any side-reported by the patient is important.
Documentation of Findings
The ultrasound findings should be thoroughly documented in still images and video clips. Images should include measurements of any masses or abnormalities along with comparisons of the contralateral side. Notation is made regarding vascularity and spectral waveform patterns if Doppler is performed. Any suspicious findings are highlighted for the interpreting radiologist.
Normal Appearances
On ultrasound, normal testicular tissue appears homogenously hypoechoic compared to the echogenic mediastinum area centrally. This mediastinum contains small tubules and vessels that may appear slightly heterogeneous. discrete foci of calcifications representing microliths may also be present.
The size of the testicle varies depending on the patient age, ranging from about 1.5 x 0.7 x 1.2 cm in newborns to 5 x 2.5 x 3 cm in adults. Testicles in adults smaller than 2 cm in length are considered abnormally small. The epididymal head is about 6-12 mm, body is 3-6 mm, and tail is 2-3 mm in diameter.
Some normal variants in echotexture can be seen, including enlarged mediastinum, sparse calcifications, and small cysts under 5 mm. Up to two tiny hyperechoic testicular microliths can also be a normal finding. there is often mild asymmetry in testicular size with the right testicle being slightly larger. Intra-testicular vascular flow varies but is typically abundant on color Doppler imaging.
Pathologies
Many scrotal abnormalities can be evaluated with ultrasound:
Testicular Cancer
- Seminoma appears as a uniform, hypoechoic, often bulging testicular mass. Calcifications are uncommon.
- Non-seminomatous germ cell tumors are more heterogeneous, multi-cystic masses that may contain calcifications due to hemorrhage or necrosis. Tumor markers are also elevated.
- Intratubular germ cell neoplasia may appear as an enlarged area of decreased echogenicity due to dilated seminiferous tubules.
Varicocele
- Dilated veins of the pampiniform plexus appear as anechoic, serpiginous tubular structures projecting from the testicle. Size increases with Valsalva maneuver.
Hydrocele
- Anechoic fluid collection surrounding the testicle separates it from the inner scrotal wall. May be communicant with peritoneal cavity.
Spermatocele
- Fluid filled cyst adjacent to the epididymis containing sperm, seen as anechoic cystic structure with thin walls and posterior acoustic enhancement.
Torsion
- Enlarged, hypoechoic testicle due to edema from loss of arterial supply. Absent intratesticular blood flow on Doppler confirms diagnosis.
Inflammation/Infection
- Orchitis: enlarged heterogeneous testicle and epididymis with hypervascularity
- Epididymitis: enlarged, hypoechoic epididymis with scrotal wall thickening
Trauma
- Testicular rupture appears as an irregular contour or heterogeneous echotexture. Extra-testicular hematoma and hydrocele can occur.
Undescended Testis
- Non-visualization indicates an abdominal undescended testis. Ectopic testes may be found along the normal descent path. Increased risk of malignancy.
Microlithiasis
- Multiple tiny intratesticular calcifications. Associated with testicular cancer in some cases.
Report Writing
The ultrasound report should include detailed descriptions of the testicles, epididymis, skin, and scrotal contents. All structures and organ borders should be evaluated and reported.
Size measurements are important for detecting any enlargement or atrophy. Side-to-side size comparisons help identify asymmetry. Any focal abnormalities, calcifications or cystic regions should be measured in 3 dimensions.
Echotexture and vascularity is noted, along with any color flow or Doppler findings. Any abnormal spectral waveforms are documented.
Comparison views to prior exams is extremely helpful to delineate subtle changes. Serial measurements of masses help determine tumor growth rates.
Succinct impressions that can be understood by referring providers are key. Follow up recommendations should be indicated based on the suspected diagnosis. Clear communication with the ordering physician ensures proper patient care and management.
Limitations
While ultrasound provides excellent anatomic detail, there are some limitations to consider:
- Operator dependence - Results can vary based on experience and skill.
- Large patient size - Obese patients may have suboptimal imaging due to body habitus.
- Gas/feces - Bowel gas shadows may obscure visualization of deeper anatomy.
- Previous surgery/radiation - This can alter the typical sonographic appearance.
- Non-palpable testes - Cannot assess non-descended abdominal testicles.
- Acute pain - Severe pain or swelling may preclude adequate compression to see internal structures.
Close correlation between ultrasound findings and the clinical scenario is always important. Further imaging like MRI may be needed if the ultrasound is non-diagnostic. CT should be avoided in younger patients due to radiation risk.
Testicular ultrasound is a quick and reliable technique to evaluate scrotal diseases and masses. It provides exceptional anatomic detail without ionizing radiation. Ultrasound should be considered a first line modality for assessment of pain, swelling or palpable abnormalities of the scrotum. With a systematic scanning approach, most intratesticular and paratesticular processes can be characterized and monitored over time. Diagnosing testicular cancers at an early stage portends a better prognosis. Testicular ultrasound is an indispensable tool for men's health.
Content Information
We review all clinical content annually to ensure accuracy. If you notice any outdated information, please contact us at info@iuslondon.co.uk.
About the Author:

Yianni is a highly experienced sonographer with over 21 years in diagnostic imaging. He holds a Postgraduate Certificate in Medical Ultrasound from London South Bank University and is registered with the Health and Care Professions Council (HCPC: RA38415). Currently working at Barts Health NHS Trust, Yianni specialises in abdominal, gynaecological, and obstetric ultrasound. He is a member of the British Medical Ultrasound Society (BMUS), Society of Radiographers (SoR) and regularly contributes to sonographer and junior radiologists training programs.