Ovarian cancer is a complex and often silent disease, making early detection critical for effective treatment. Understanding how pelvic ultrasounds assist in detecting ovarian abnormalities, including cancer, can give patients reassurance and clarity about the screening process. In this article, we’ll examine what ovarian cancer entails, how pelvic ultrasounds work, and what findings may suggest a need for further examination.

What is Ovarian Cancer?
Ovarian cancer arises from abnormal cell growth in the ovaries. The three primary types of ovarian cancer are epithelial, germ cell, and stromal tumors, with epithelial being the most common. This disease is known for its subtle early symptoms, often leading to later-stage diagnoses. Risk factors include age (typically affecting women over 50), family history, genetic predispositions (such as BRCA1 and BRCA2 gene mutations), and certain reproductive history factors.
Symptoms may start mildly but often include bloating, pelvic pain, difficulty eating, and urinary symptoms, which are easy to overlook or attribute to less serious conditions. The asymptomatic nature of ovarian cancer at its onset underscores the importance of proactive screening methods like ultrasound to detect signs before symptoms become advanced.
What is a Pelvic Ultrasound?
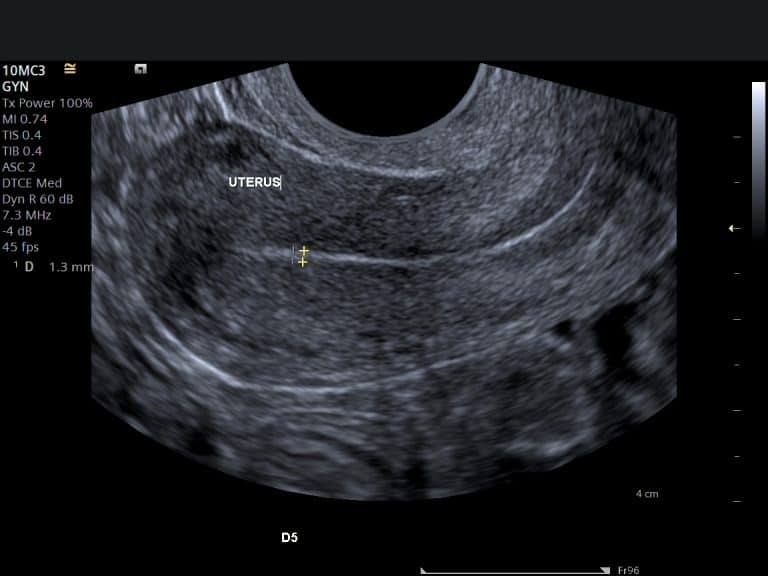
A pelvic ultrasound is a diagnostic imaging tool that uses high-frequency sound waves to create images of structures within the pelvis. Ultrasound is valued in gynecologic imaging because it’s non-invasive, does not use radiation, and provides a clear picture of soft tissues, including the ovaries. Pelvic ultrasound can be performed in two ways: transabdominally or transvaginally, each offering distinct advantages.
Transabdominal Ultrasound
This method involves placing a probe over the lower abdomen, offering a broad view of the pelvic organs. It’s commonly used when scanning larger areas or in patients who may be uncomfortable with transvaginal approaches, such as those who are pregnant. While effective, transabdominal ultrasound can sometimes miss smaller ovarian abnormalities that transvaginal imaging would detect.
Transvaginal Ultrasound
For a more detailed image of the ovaries and surrounding structures, transvaginal ultrasound is often preferred. A specialized probe is gently inserted into the vaginal canal, providing close-up images of the ovaries. This proximity allows for higher-resolution images, making it easier to identify smaller lesions or cysts and assess their characteristics. Research shows that transvaginal ultrasound is especially useful in detecting early-stage ovarian tumours due to its detailed imaging capabilities.

How Pelvic Ultrasound Detects Ovarian Abnormalities
Pelvic ultrasound allows radiologists to examine the ovaries’ size, shape, and internal structure. By analyzing these aspects, radiologists can identify abnormalities like cysts or solid masses. Cysts, which are often benign, appear as fluid-filled sacs, while solid masses, especially those with irregular borders, warrant closer examination due to the potential association with malignancy.
Studies show that certain ultrasound features, like irregular shape, internal septations, and solid components, can indicate higher risk. For instance, a solid, irregular mass with increased vascular flow, observed through Doppler ultrasound, raises suspicion and may require further testing. Research published in the American Journal of Obstetrics & Gynecology confirms that Doppler ultrasound, which assesses blood flow patterns, is instrumental in distinguishing benign from malignant ovarian masses by evaluating the amount of blood flowing to the area.
Ultrasound Features Suggestive of Ovarian Cancer
Ovarian cancer tends to present certain characteristics on ultrasound that help differentiate it from benign conditions. Here are some key findings:
Solid Masses: Unlike benign cysts, malignant tumors often contain solid tissue. Studies indicate that solid components, especially in complex cysts, are more likely to suggest malignancy.
Irregular Borders: Cancers usually present with irregular, lobulated borders rather than the smooth, round edges typically seen in benign cysts. This feature can be a red flag in identifying suspicious ovarian masses.
Septations and Nodules: Internal septations (thin walls within a cyst) or nodules attached to the walls may point to a more complex and potentially malignant nature. Research has consistently shown that the presence of nodules or thick septations increases the likelihood of cancer.
Increased Vascularity: Blood flow in tumors is often more prominent than in benign lesions. Doppler ultrasound can highlight this increased blood supply, which is commonly seen in malignancies.
A comprehensive review of ultrasound features published in the journal Radiology highlighted that using a combination of these characteristics provides a higher accuracy rate in identifying malignant ovarian masses. Radiologists interpret these findings within the context of patient history and risk factors, offering a nuanced approach to diagnosis.
The Role of Ultrasound in Ovarian Cancer Diagnosis and Staging
While ultrasound is a primary tool in detecting ovarian abnormalities, it’s part of a larger diagnostic process. If ultrasound findings are suspicious, additional testing such as blood tests (e.g., CA-125) or other imaging studies (CT or MRI) may be recommended for a clearer picture. Studies published in the International Journal of Gynecologic Cancer suggest that ultrasound, combined with CA-125 testing, provides higher predictive value, particularly in postmenopausal women. This combination allows clinicians to differentiate between malignant and benign conditions with greater precision.
Ultrasound also plays a role in staging ovarian cancer by assessing the extent of tumor spread within the pelvic area. Although CT scans and MRIs are more commonly used for detailed staging, ultrasound remains valuable for tracking tumor response to treatment and identifying residual disease after surgery.
What to Expect During a Pelvic Ultrasound for Ovarian Cancer Screening
For patients, understanding the procedure can reduce anxiety. During a transabdominal ultrasound, the patient lies on an examination table while a clear gel is applied to the abdomen to help transmit sound waves. The technician moves a probe across the abdomen, capturing images. Patients are usually asked to have a full bladder, as this enhances image clarity.
In a transvaginal ultrasound, a slender probe covered with a disposable cover and lubricating gel is inserted into the vaginal canal. This approach offers a close-up view of the ovaries. The procedure is generally painless, though some may experience mild discomfort. Transvaginal ultrasound often takes 15-30 minutes, with real-time image capture allowing immediate analysis by the radiologist.
Frequently Asked Questions (FAQs) about Pelvic Ultrasound and Ovarian Cancer
Can a pelvic ultrasound definitively diagnose ovarian cancer?
While pelvic ultrasound is highly effective at identifying suspicious features, it cannot definitively diagnose ovarian cancer. Confirmation requires additional testing, such as biopsy or advanced imaging, depending on the initial findings.
Is a pelvic ultrasound painful?
A pelvic ultrasound is typically a comfortable procedure. Transabdominal ultrasound involves only external pressure, which most patients tolerate well. Transvaginal ultrasound may feel mildly uncomfortable, but pain is uncommon. Open communication with the technician about comfort levels ensures a smooth experience.
How long does it take to receive results?
Results are usually available within a few days. A radiologist reviews the images, assessing for abnormalities. If findings require further exploration, the radiologist will work with the referring physician to outline next steps.
How often should I have an ultrasound if I’m at high risk?
For individuals with a family history of ovarian cancer or genetic predispositions, doctors may recommend annual ultrasounds as part of a surveillance program. Studies on high-risk groups, such as those with BRCA mutations, indicate that regular ultrasound screenings improve early detection rates, helping to catch potential issues at more treatable stages.
Summary and Key Takeaways
Pelvic ultrasound is a reliable and non-invasive approach for visualizing ovarian structures, helping identify abnormalities that could indicate ovarian cancer. Through advanced imaging techniques, radiologists can assess size, shape, and vascularity, offering early insight into potential issues. For patients, understanding this process can ease concerns and encourage proactive health care steps.
A pelvic ultrasound is more than just a diagnostic procedure—it’s a critical tool in detecting ovarian abnormalities early and supporting patients on their journey to understanding their reproductive health. By knowing what to expect and recognizing the importance of ultrasound in early detection, patients can approach their care with greater confidence and clarity.