Experiencing abnormal bleeding can be distressing, and understanding what may be causing it is essential for peace of mind and proper care. One of the most effective diagnostic tools used to investigate abnormal bleeding is the pelvic ultrasound. This imaging technique provides valuable insights into what might be happening internally, offering a non-invasive way to diagnose a range of conditions that could be contributing to the bleeding.
What is Abnormal Bleeding?
Abnormal bleeding includes any bleeding that deviates from a regular menstrual pattern or occurs outside of the usual menstrual cycle. This can include heavy menstrual bleeding, irregular cycles, postmenopausal bleeding, or bleeding between periods. Many underlying factors can contribute to abnormal bleeding, including hormonal imbalances, fibroids, polyps, or structural issues within the uterus or ovaries.
When bleeding patterns shift significantly, it often warrants investigation through imaging techniques like pelvic ultrasound, which allows healthcare providers to explore potential causes without the need for surgical intervention.

Why Use Pelvic Ultrasound?
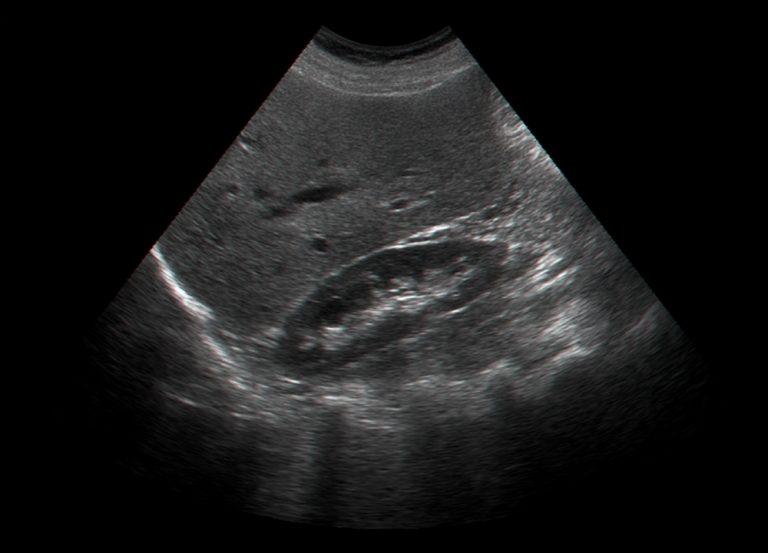
Pelvic ultrasound is widely used to assess various gynecological conditions, including the causes of abnormal bleeding. This imaging method is favored for several reasons: it’s safe, does not use ionizing radiation, and can provide real-time images that help identify structural abnormalities in the uterus, ovaries, and surrounding tissues.
Healthcare providers often recommend pelvic ultrasound as a first-line imaging technique for patients presenting with abnormal bleeding because it can efficiently highlight a range of conditions, from benign growths like fibroids to more complex issues such as endometrial thickening or ovarian cysts. This diagnostic process plays a key role in creating a tailored treatment approach for each patient, based on specific ultrasound findings.
Types of Pelvic Ultrasound
Pelvic ultrasound comes in two main types: transabdominal and transvaginal. Both serve different purposes and offer unique advantages, depending on what needs to be examined.
Transabdominal Ultrasound
A transabdominal ultrasound involves placing the ultrasound probe on the lower abdomen, typically while the patient has a full bladder. A full bladder provides a “window” that improves image clarity by pushing the intestines away from the pelvic organs, making it easier to visualize the uterus and ovaries.
This method is especially useful for giving an overall view of the pelvic region and is often the initial approach for patients presenting with pelvic symptoms, as it offers a broader overview.
Transvaginal Ultrasound
Transvaginal ultrasound provides higher-resolution images of the uterus, endometrium, and ovaries. This method involves inserting a slender ultrasound probe into the vaginal canal, allowing closer proximity to the pelvic organs.
Transvaginal ultrasound is particularly helpful for examining the endometrium, which is often the source of abnormal bleeding, especially in postmenopausal patients. This approach can reveal details about endometrial thickness, small polyps, and early stages of certain conditions that may not be visible in a transabdominal scan.
What to Expect During a Pelvic Ultrasound
Understanding the process of a pelvic ultrasound can make the experience smoother and more comfortable. Both transabdominal and transvaginal ultrasounds are generally straightforward and don’t require extensive preparation.
Preparing for the Ultrasound
For a transabdominal ultrasound, patients are typically advised to drink several glasses of water before the procedure, as a full bladder helps achieve clearer images. For transvaginal ultrasounds, no specific preparation is needed, though some patients may feel more comfortable if they empty their bladder beforehand.
During the Ultrasound
During a transabdominal ultrasound, patients lie back while the sonographer applies a water-based gel on the abdomen and glides the ultrasound probe over the area. This process is painless, though slight pressure may be felt as the probe moves over certain regions.
In a transvaginal ultrasound, the probe, about the width of a tampon, is gently inserted into the vaginal canal. This procedure is also generally comfortable, though it may cause mild pressure. Sonographers are highly skilled in ensuring patients feel as at ease as possible during this part of the examination.
How Pelvic Ultrasound Helps Identify Causes of Abnormal Bleeding
The images generated by a pelvic ultrasound allow healthcare providers to evaluate potential causes of abnormal bleeding. Different findings from a pelvic ultrasound can point to various underlying issues.
Uterine Fibroids and Polyps
Uterine fibroids are non-cancerous growths that develop in the muscle tissue of the uterus. Fibroids vary widely in size and number and can distort the shape of the uterus, contributing to heavy bleeding, prolonged periods, and pelvic pain. According to the American College of Obstetricians and Gynecologists, fibroids are common and often occur in women of reproductive age. Polyps, on the other hand, are growths that develop in the lining of the uterus and can also lead to abnormal bleeding, especially between periods.
Ultrasound imaging shows the size, location, and number of fibroids or polyps, helping to guide treatment options that range from medication to surgical removal if symptoms are severe.
Endometrial Abnormalities
The endometrium, or the lining of the uterus, plays a key role in regular menstrual bleeding. Changes in endometrial thickness can indicate various conditions, particularly in postmenopausal women who should not typically experience bleeding. Abnormal thickening, which may suggest endometrial hyperplasia or even early signs of endometrial cancer, can be effectively evaluated through a transvaginal ultrasound.
Research published in the American Journal of Obstetrics and Gynecology has shown that transvaginal ultrasound can detect abnormalities in endometrial thickness with high sensitivity, making it a valuable tool for early diagnosis.
Ovarian Cysts
Ovarian cysts are fluid-filled sacs that develop on or inside an ovary, often during ovulation. While most cysts are benign and resolve on their own, larger cysts or those that rupture can cause symptoms like pelvic pain and irregular bleeding. Pelvic ultrasound helps determine the cyst’s size, structure, and content, providing a basis for deciding whether monitoring or intervention is necessary.
Uterine Structural Abnormalities
Some women are born with structural abnormalities in the uterus, such as a septate uterus (a uterus divided by a wall of tissue) or a bicornuate uterus (a heart-shaped uterus). These abnormalities can cause irregular bleeding, particularly if they interfere with normal menstrual flow. Pelvic ultrasound can reveal these structural issues, allowing healthcare providers to consider corrective procedures when appropriate.
Interpreting Results
After the ultrasound examination, the images are analyzed by a radiologist, who interprets the findings and generates a report. The results offer a clearer picture of any physical changes or abnormalities within the pelvic organs.
Patients often receive results through their referring healthcare provider, who explains the findings and discusses potential next steps. If the ultrasound identifies fibroids, polyps, or cysts, for example, the provider may suggest monitoring, medication, or further testing. For complex cases or findings suggestive of more serious conditions, additional diagnostic procedures, like MRI or biopsy, may be recommended.
Next Steps After the Ultrasound
Following a pelvic ultrasound, patients should discuss their results in detail with their healthcare provider. The next steps vary widely, depending on the ultrasound findings. Some patients may require no further action if the ultrasound shows normal findings, while others might need to explore treatment options.
Treatment for abnormal bleeding could include hormonal therapies, non-hormonal medications, or minimally invasive procedures like endometrial ablation. In cases where structural abnormalities or significant growths are found, surgery may be an option.
Each treatment approach aims to address the root cause of the abnormal bleeding, and having clear ultrasound results helps providers personalize care to the patient’s unique needs.
Frequently Asked Questions
Is the Procedure Painful?
Pelvic ultrasound is generally a comfortable procedure. Patients may feel mild pressure during a transabdominal ultrasound or slight discomfort during a transvaginal ultrasound, but significant pain is rare.
How Long Does It Take?
Most pelvic ultrasounds take around 10-15 minutes, although the exact time can vary. The sonographer will usually let the patient know what to expect beforehand.
Will Results Be Available Immediately?
In most cases, the sonographer captures the images during the ultrasound, and a radiologist reviews them later. This means patients typically receive their results within a few days from their healthcare provider.
What If the Ultrasound Is Normal, But Symptoms Persist?
A normal ultrasound result does not always rule out all causes of abnormal bleeding. If symptoms continue, further evaluation may be needed, and healthcare providers may consider other diagnostic options.
Final Thoughts
A pelvic ultrasound is a valuable diagnostic tool for uncovering the causes of abnormal bleeding. It provides crucial information about the structure and health of pelvic organs, guiding appropriate and effective treatment options. Patients who understand the procedure and what to expect can approach their care with confidence, knowing they are taking essential steps toward better health.