Follicular tracking scans, also known as fertility monitoring scans, are an important part of fertility treatments like IVF and IUI. They allow your doctor to closely monitor your ovarian follicles during your treatment cycle.
The scans track the growth and development of follicles in your ovaries. Follicles are fluid-filled sacs that contain the eggs. Tracking follicular growth allows your doctor to pinpoint the optimal time for egg retrieval or insemination.
Understanding your follicular tracking scan results is key. This guide will explain:
- What a follicular tracking scan entails
- How to interpret follicular tracking scan results
- Follicle size
- Follicle number
- Lining thickness
- Estrogen levels
- What ideal scan results look like at different points in your cycle
- Potential issues identified by tracking scans
- Next steps after your scan
What Does a Follicular Tracking Scan Entail?
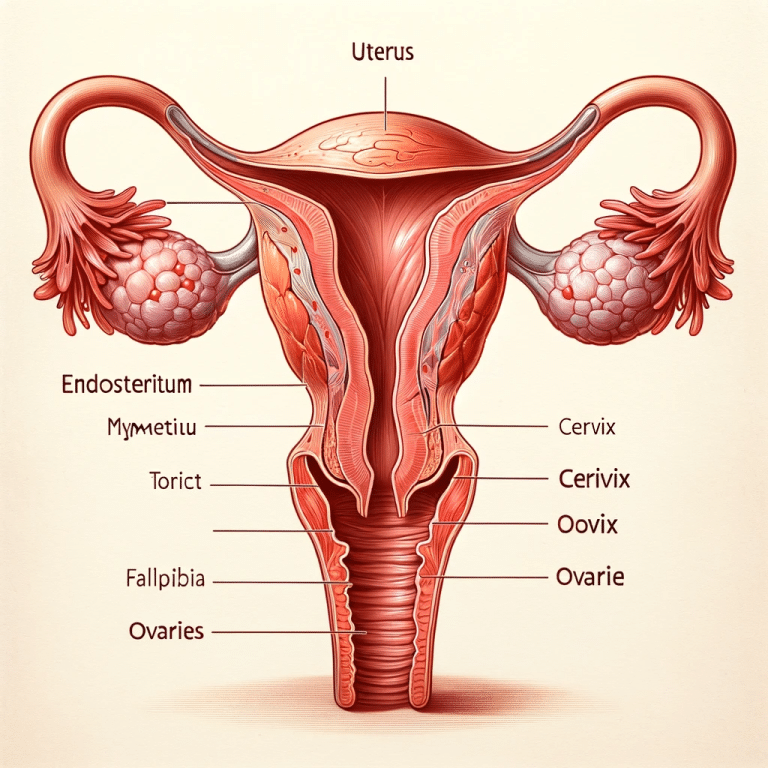
Follicular tracking scans use vaginal ultrasounds to visually inspect your ovaries and measure your follicles. The probe is inserted into the vagina to get closer to the ovaries for better visualization.
During the ultrasound, your doctor will measure the size and count the number of follicles developing in your ovaries. They will also measure the thickness of your endometrial lining.
Tracking scans are typically performed every 1-3 days at the start of your treatment cycle. Your doctor will monitor how your follicles are responding to the fertility medications you are taking.
Once the follicles reach a mature size, your final scan will indicate the ideal timing for your egg retrieval or ovulation trigger shot. This is known as your “trigger scan”.
Some clinics also perform blood tests on the day of your scan to measure estrogen levels. Estrogen rises as the follicles grow, so blood levels provide additional data.
How to Interpret Follicular Tracking Scan Results
There are four key parameters your doctor will evaluate during your tracking scans:
Follicle Size
- Follicle size indicates the stage of egg maturation. Bigger follicles contain more mature eggs.
- Most clinics look for follicles to reach 16-22mm before egg retrieval or ovulation.
- Follicles are measured across their widest diameter. Your report may provide an average or a range.
- Too small – Immature eggs. Need longer stimulation.
- Too big – Overly mature eggs. Risk of spontaneous ovulation.
Follicle Number
- The number of follicles reflects your ovarian reserve and response to medications.
- A higher number of mature-sized follicles means more eggs can be retrieved.
- 10 or more follicles is considered a good response. Less than 3 is a low response.
- Too few – May indicate low ovarian reserve or poor stimulation.
- Too many – Risk of ovarian hyperstimulation syndrome (OHSS)
Lining Thickness
- The endometrial lining must thicken to support embryo implantation.
- Lining is measured from the outer edge across the full width.
- Ideal thickness is usually 8mm or greater by trigger day.
- Too thin – May prevent embryos from implanting.
- Too thick – Can happen in women with PCOS. Can also impair implantation.
Estrogen Levels
- Estrogen levels rise as follicles develop and increase in size.
- Levels are measured in pg/mL or pmol/L.
- There is a wide range of “normal” based on the phase of your cycle.
- Your clinic will be looking for levels to rise steadily over your monitoring period.
- High levels may indicate OHSS risk. Low levels may reflect poor response.
What Do Ideal Scan Results Look Like?
Follicle and lining measurements will vary throughout your treatment cycle as you progress from medications to ovulation/retrieval. Here’s what to expect:
Baseline Scan
- Performed at the start of your treatment cycle before medications begin
- Determines antral follicle count (AFC) – the number of resting follicles in your ovaries
- Confirms ovaries are quiet with no dominant follicles and thin lining
- Estrogen levels will be low
After 5-7 Days of Stimulation
- Early follicular development with follicles around 10mm
- Potential lead dominant follicle of 12mm or more
- Lining thickening to around 5mm
- Rising estrogen levels
Final Scan Before Trigger
- Multiple mature follicles 16-22mm
- Leading follicles ≥18mm preferred
- Lining thickness ≥8mm triple striped pattern
- Estrogen levels consistent with follicle growth
These results indicate you are ready to proceed with egg retrieval or your ovulation trigger shot.
Your ideal results will depend on your age and diagnosis. Your doctor will be looking for an appropriate response to your protocol.
Potential Issues Identified by Tracking Scans
Follicular tracking allows your doctor to monitor your cycle for potential problems like:
- Poor Response: Few or no follicles growing with low estrogen levels. Indicates low ovarian reserve.
- Over Response: Too many follicles developing rapidly. Puts you at risk of OHSS.
- Premature Luteinization: LH surge before trigger leading follicles to luteinize early. Risk of oocyte maturation.
- Thin Lining: Inadequate endometrial thickening. Prevents embryo implantation.
- Cysts: New cysts may require freezing all embryos and converting the cycle to IUI or cancelation.
Your doctor will discuss any issues seen on your scan and recommend protocol adjustments as needed.
Next Steps After Your Follicular Tracking Scan
Your doctor will review your follicular development, lining thickness, estrogen levels, and any issues identified on your scan. They will then advise the next steps:
- Continue Monitoring: If follicles are still growing, you will return in 1-3 days for your next scan to track continued progress.
- Adjust Medications: Changes in medication dosing may be made to improve follicle growth and development or prevent over-response.
- Schedule Retrieval/Trigger: When follicles have reached maturity, retrieval or trigger will be scheduled within the next 36 hours.
- Cycle Cancellation: Your doctor may stop the cycle if there are too few follicles, poor lining, or excess risk of complications like OHSS.
- Freeze All: If the follicular response is excessive or other issues arise like premature luteinization, freezing all embryos may be recommended. A frozen embryo transfer can be performed later with proper hormonal priming.
Understanding what to look for in your follicular tracking scan results will help you know what to expect throughout your IVF or IUI cycle. Discuss your results thoroughly with your doctor and don’t hesitate to ask questions. Tracking your follicle growth and cycle response empowers you to be an informed and engaged patient.
Frequently Asked Questions
How many follicular tracking scans will I need?
Most patients undergo 3-5 tracking scans per cycle. After your baseline scan, you will typically have scans every 1-3 days to monitor follicle growth until the lead follicles reach maturity. The number can vary based on your ovarian response and cycle details.
Do follicular tracking scans hurt?
The transvaginal ultrasound probe can cause mild discomfort, pressure or brief pain as it is inserted and maneuvered to visualize your ovaries. Many women do not find the scans painful, but taking ibuprofen an hour before your appointment can help. Let your doctor know if you experience significant pain so they can be as gentle as possible.
Why are higher estrogen levels concerning during IVF stimulation?
High estrogen levels can indicate that too many follicles are developing rapidly. This excessive response puts you at higher risk of ovarian hyperstimulation syndrome (OHSS) if all embryos are transferred. Your doctor may recommend freezing all embryos and doing a frozen transfer in a subsequent cycle with hormone replacement.
How do I know if my follicles are growing too slowly or too fast?
Your doctor monitors the number of follicles and their growth from scan to scan. 1-2mm per day is considered normal growth. If growth stalls, your doctor may increase medications. Excessive growth of 3+ follicles rapidly to over 18mm indicates overresponse and OHSS risk.
What happens if my follicles are too small on the final scan?
If lead follicles remain under 14mm and estrogen levels are low, your doctor will likely have you continue stimulation for a few more days. If there is still inadequate response, the cycle may be cancelled as the eggs are unlikely to be mature. The protocol can be adjusted to improve response for your next cycle.
When should I trigger if my follicle size is borderline?
Some follicles may be borderline maturity between 15-18mm on your final scan. Your doctor will assess your estrogen levels, the number of mature follicles, lining thickness and past response. If estrogen is rising appropriately and most follicles are >15mm, they may recommend proceeding with trigger for borderline results.
Can I get pregnant naturally the cycle after an IVF cycle?
Yes, you may ovulate as soon as two weeks after your IVF cycle is completed. It is possible to conceive naturally if you engage in unprotected intercourse during this period. Many clinics recommend birth control after IVF if you wish to prevent pregnancy in the cycle immediately after.
How will my doctor adjust medications for a thin lining?
If your lining is under 7mm on your final scan, your doctor may prescribe vaginal estradiol or Viagra suppositories to quickly thicken the lining before transfer. Intramuscular estradiol injections or extended time on oral estrogens may be used for a new stimulation cycle to achieve a thicker lining.
When would my doctor cancel my IVF cycle?
Cycle cancellation most commonly occurs due to poor ovarian response resulting in just 1 or 2 follicles. This provides a low chance of success. Risks like OHSS or inadequate lining may also lead to cancellation. Your doctor will discuss the reasoning and options like changing medications or doing another retrieval after a period of rest.
The Takeaway
Monitoring your follicular development with vaginal ultrasounds and bloodwork is a vital part of fertility treatments like IVF and IUI.
Look for your follicles to grow 1-2mm daily to a mature size over 16mm. Your lining should thicken to over 8mm. Estrogen levels will rise as follicles develop.
Discuss your results thoroughly with your doctor. Track your progress but avoid fixating on small differences. Focus on the overall trajectory.
Understanding your response to medications allows optimization of treatment for the best possible egg quality and cycle success. Work as a team with your doctor and trust their guidance through this process.