Pelvic Ultrasound Results Explained.
If you had a pelvic ultrasound scan and you are reading your ultrasound report you are probably wondering what is all about as ultrasound reports can be very confusing sometimes.
Read below, where we are trying to explain the most common terminology that might be used in your report.
Why would a doctor order a pelvic ultrasound?
If you have been experiencing painful periods, unusual vaginal bleeding, chronic pelvic pain, or are having difficulty conceiving, your doctor may recommend a pelvic ultrasound. This test is a safe, non-invasive way for your doctor to obtain more information to make an accurate diagnosis and offer appropriate options for infertility treatment.
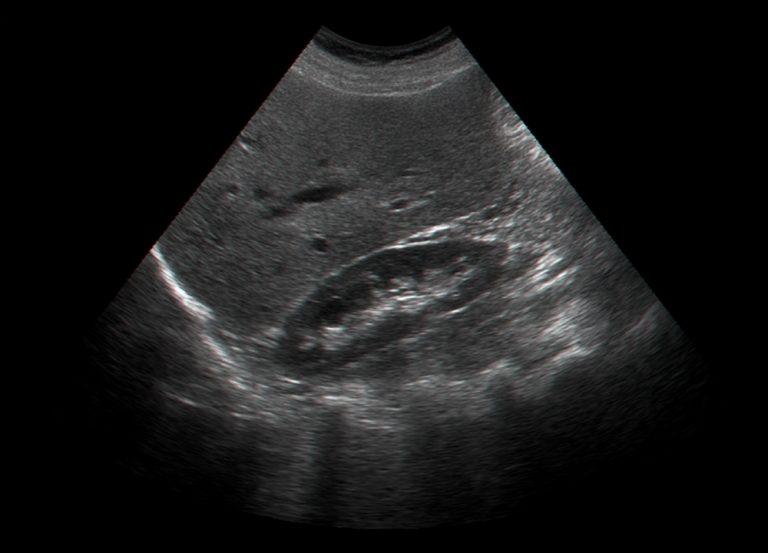
Ultrasound or sonography uses sound waves to produce an image of organs and other tissues in the body. Gynaecological ultrasounds are helpful for identifying abnormalities of the reproductive organs such as uterine fibroids or ovarian cysts and can assist your doctor to determine appropriate infertility treatment options. Ultrasounds are also used during pregnancy to monitor the growth of the unborn baby. Another advantage of having an ultrasound is that there is no risk of potentially harmful radiation as with an x-ray.
You can find more information about pelvic ultrasound on our blog pages and learn more about the private pelvic scan we offer in London on our dedicated exam page.
The ultrasound Report
A gynaecological scan ultrasound report will include information about the:
- Uterus
- Endometrium
- Ovaries
- Surround areas
A basic ultrasound report reads like this:
“The anteverted uterus is of normal size, shape, outline and echotexture.
A fundal subserosal fibroid is noted, measuring 25 mm.
The endometrium is smooth and regular in outline, measuring 10 mm at the fundus. (LMP Day 16).
Both ovaries are normal in ultrasound appearances. No ovarian cysts seen.
No adnexal masses identified. No free fluid seen within the pelvis.”
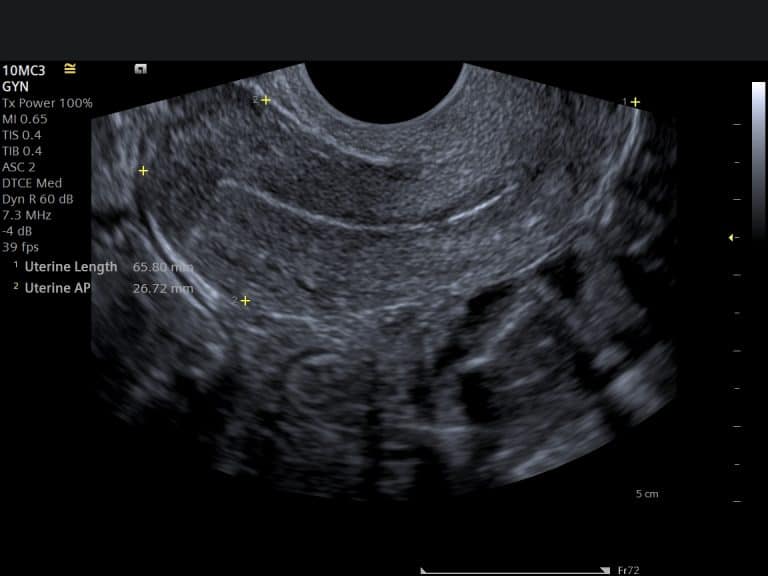
The uterus
The report will describe the position of the uterus, for example, anteverted, retroverted, axial etc. The most common presentation is anteverted (around 80%) which means pointing upwards.
Retroverted means pointed backwards, and in the axial position, the uterus points towards the head (superior).
The report will mention the size of the uterus will be commented either subjectively i.e ‘The uterus is normal size’ or objectively for example, ‘The uterus measures x cm.
The normal size of a uterus is around 6-10 cm in length and 3-5 cm in depth.
Echotexture or echopattern describes the ultrasound appearance of the uterus. The appearance can be normal or heterogeneous due to some myometrial pathology, for example fibroids or adenomyosis.
Fibroids are one of the most common uterine abnormalities and are classified as subserosal, submucosal, intramural and pedunculated according to their location.
You can read more about ultrasound for uterine fibroids in our other blog article.
Adenomyosis is another pathology affecting the myometrium. This is when a part of the endometrium (the lining of the womb) plants itself in the myometrium.
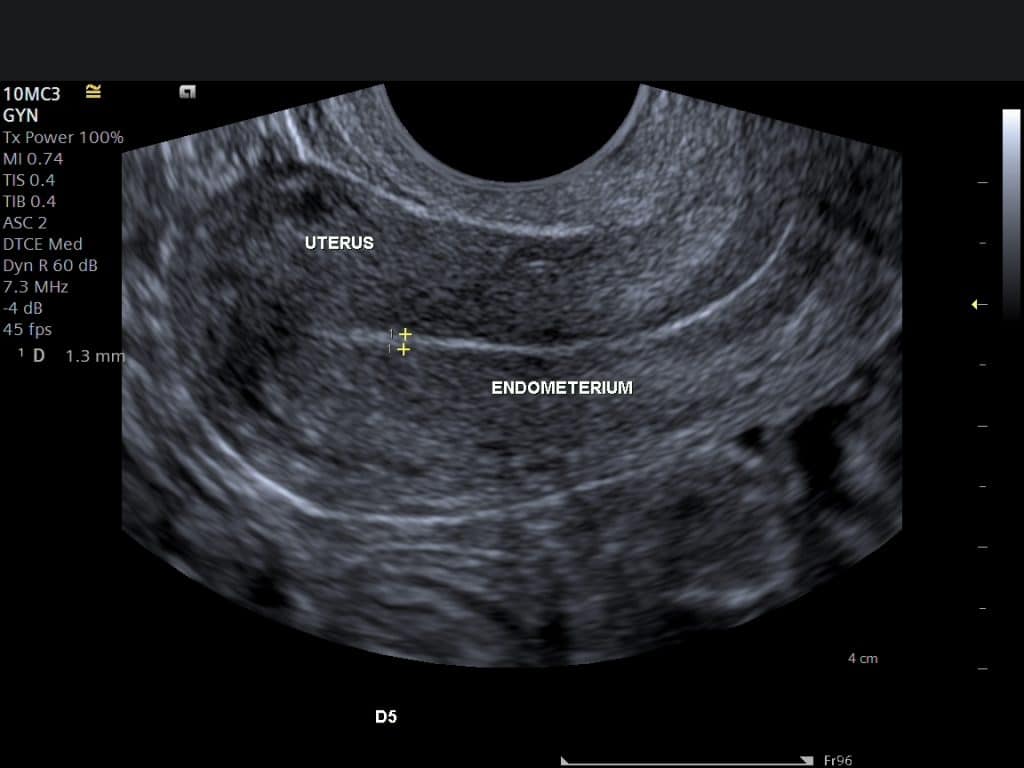
The endometrium
The endometrium is the lining of the womb.
The ultrasonic appearance of the endometrium is described, as well as the thickness that hopefully will correlate with the day of the cycle.
The thickness of the endometrium depends on the stage of the cycle and can be from 1-14 mm.
The abnormal thickness of the endometrium can be due to polyps, submucosal fibroids, hyperplasia and cancer.
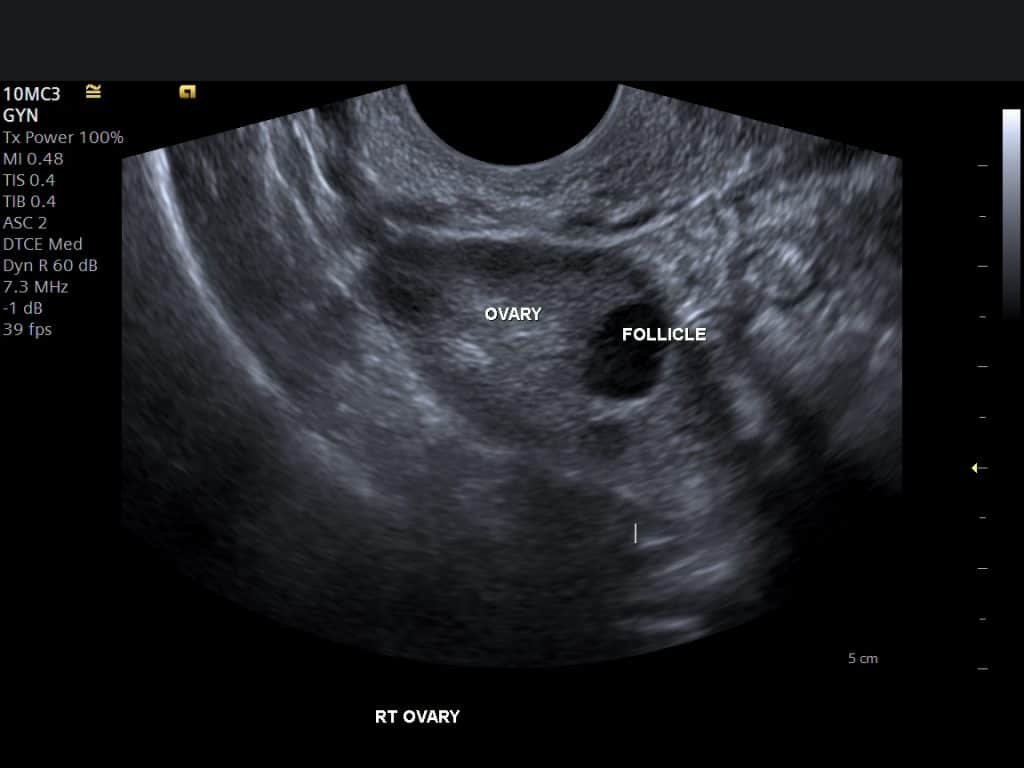
The ovaries
The ultrasound report will describe the appearance of the ovaries and the size or volume of the ovaries. The normal ovarian volume is 1.2-9.4 cm3.
The report will include information on any cysts present such as follicular cysts, corpus luteum cysts, haemorrhagic cysts, endometriomas, simple cysts and polycystic appearing ovaries.
Sometimes the ovaries can not be seen on a scan, which is reassuring as it excludes pathology.
Surrounding areas
During the scan, which can be performed transabdominal or transvaginal, the sonographer will evaluate the surrounding areas called adnexae and pouch of Douglas for any abnormality and the presence of any free fluid.
The fallopian tubes are not normally visible on an ultrasound scan unless they are abnormally distended by fluid and in most cases a hydrosalpinx or pyosalpinx.
References
1. Eberhard Merz. Ultrasound in Obstetrics and Gynaecology. Vol. 2. 2nd edition, Thieme, Texas, 1997.
2. Goldberg BB, McGahan JP. Atlas of Ultrasound Measurements. Elsevier Health Sciences, Philadelphia 2006.
3.SIGN. Investigation of post-menopausal bleeding. SIGN guideline 61, 2002